Are you avoiding social events because of your heavy period? Missing work? Soaking through a great outfit, or your mattress? How about getting on birth control for your wedding to avoid a blood bath on your special day?
If you have heavy periods, they can be very inconvenient. They can also be exhausting.
I always say that your period blood isn’t ‘extra blood’, it’s real substance that your body made with work and nutrients. And it’s work to make it all over again. Now, if you health is good and your flow is normal, it’s all good. But when your flow is excessive, you can end up depleted.
This article will help define what a heavy period is, why it happens, and some great ideas on what to do about it. So let’s get started!
1. How Much is Too Much Menstrual Bleeding?
The range of normal flow is 10-60 ml, according to the National Health Service of the UK.
According the Centre for Menstrual Cycle and Ovulation Research, the average flow a woman has is 30 ml, or 2 Tablespoons. It doesn’t sound like much, but it’s 6 soaked tampons or pads. Considering that most women will have a heavy day or two, and a few light days (4-6 days in total), this sounds about right.
Over 60 ml or over 80 ml (depending who you ask), i.e. 16 soaked menstrual pads, is considered menorrhagia- very heavy menstrual bleeding often with clots and flooding. Women in last category will often experience iron-deficient anemia (inadequate red blood cell count).
While it’s normal to have a heavy day or two, if you have to always pair a tampon with a pad, or re-arrange your schedule around your flow, it’s too much. If you have heavy multiple heavy days, like 4+ heavy days, it’s also too much. If you find yourself very exhausted and short of breath due to your period, these are further symptoms.
2. What Causes Excess Menstrual Bleeding?
The most common reason for heavy bleeding is estrogen dominance. First let’s define estrogen, and how it affects your cycle.
Estrogen is a hormone that influences many processes in your body, from bone formation to clear thinking. Estrogen is mainly made in the ovaries, although it can also be made by the adrenal glands or in your fat tissue.
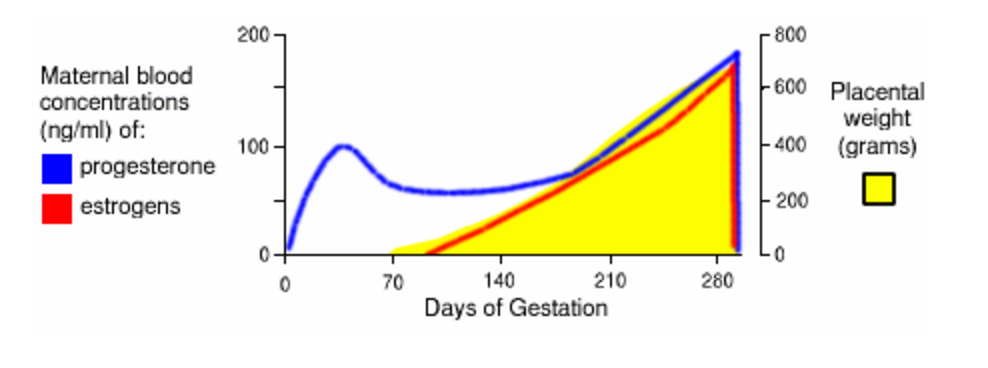
Each time you have a period, your hormone levels drop. When they drop, the brain registers this change and signals your ovaries to make more estrogen. This estrogen ripens a new egg for the next period cycle, and the estrogen grows your uterine lining.
This growth phase is fairly short. You have your period for 4-6 days (ideally), and then your build the lining up for about another ten days. At day 14 (ideally), you ovulate. While you continue to make estrogen, another hormone, progesterone, becomes the dominant player after ovulation. The progesterone firms up and matures your uterine lining, making it hospitable for a potential pregnancy.
Now let’s say this ideal picture is disturbed by too much estrogen, or not enough progesterone to balance out the estrogen. Then you get more growth in you uterine lining. This means more blood at period time, and can lead to big clots too.
There are lots of reasons for estrogen dominance. Not all of them will apply to you (: So I’m giving a clear heading for each type, so you can scan over them and see which may be a match for you. In section three, we’ll cover ways to address these issues, so keep reading!
A. You Are Getting Your First Periods
When you have your first period as a young woman, estrogen levels pump up! As your ovaries come to life, your brain and ovaries learn how to dance together, and your first few years of cycling can be irregular. Heavy, painful periods are commonly reported in teenage women.
This does not mean you have to just accept your fate or get on birth control pills. Many young women have a poor diet and are being exposed to chemicals and growth hormones. Please see the ‘What Can You Do About Heavy Bleeding?’ section for tips!
B. You are Overweight
Your fat cells house an enzyme called aromatase, used in the manufacture of estrogen. The higher your percentage of body fat, the more estrogen you can produce. As you reduce stored body fat, your estrogen production will lessen as well. Ironically, when you lose weight you will release estrogen that was stored in that fat tissue, and you can become more hormonally imbalanced in the process. So lose weight at a moderate pace.
As you age, the lowered amount of estrogen you produce can slow your metabolism and lead to more weight gain, especially in the middle. Conversely, the amount of estrogen you produce in your fat and other peripheral locations can cause an estrogen overload and heavy periods. Sometimes it’s just not fair! (Source)
C. You are Exposing Yourself to Chemicals and Food Additives
Before I became educated, I would look at my shampoo bottle and its list of chemical ingredients and think, “well I’m sure these are safe for me or they wouldn’t be in here.” Nope.
According to a 2013 article in the NY Times, “In its history, the E.P.A. has mandated safety testing for only a small percentage of the 85,000 industrial chemicals available for use today. And once chemicals are in use, the burden on the E.P.A. is so high that it has succeeded in banning or restricting only five substances, and often only in specific applications: polychlorinated biphenyls, dioxin, hexavalent chromium, asbestos and chlorofluorocarbons.”
Many of these chemicals are xenoestrogens, or chemical compounds that look like estrogen to the body. When these chemicals get inside of you, through eating them, rubbing them on your skin, or inhaling them, they attach to estrogen receptors in the body. That means your cells get the estrogen message, and to the uterine lining that means “grow”!
That’s why it’s so important to limit your exposure to these compounds, at any age. For a some women, these compounds could mean heavy periods. For other women, they can contribute to breast and other cancers. (Source)
D. You Have an Underactive Thyroid
Thyroid disease is skyrocketing in our culture. According to the American Thyroid Association, more than 12 percent of the U.S. population will develop a thyroid condition during their lifetime and women are five to eight times more likely than men to have thyroid problems.
Your low thyroid activity can lead to low reproductive hormone production. This can mean you don’t ovulate as often, or that you make less progesterone.
When you have low thyroid activity you also have decreased sex hormone binding globulin (SHBG), which can mean that more estrogen in circulation, leading to heavy periods. (Source)
To complicate matters, high estrogen can bind up thyroid hormone, feeding the imbalance!
E. You Are Not Ovulating
Here’s some news that most women don’t seem to know; just because you have periods doesn’t necessarily mean you are ovulating. Sometimes the body seems to be cycling, because it is trying to achieve that, but it’s kind of going through the motions.
This can be due to stress, due to being underweight or nutrient deficient, due to perimenopause, or due to polycystic ovarian syndrome (PCOS). Whatever the cause, if you don’t ovulate, then you’re going to make less progesterone (which is made after ovulation), so you won’t have that to balance out the estrogen production.
If you don’t ovulate you can also get your period in a very delayed timeline, so then the estrogen is left unchecked for even longer.
F. You Have Low Progesterone
This cause is a cousin to the ‘you are not ovulating’ cause above. Even if you do ovulate, if you ovulate a poor quality egg, or have other hormone production problems, then the estrogen is left somewhat unchecked. This may also cause spotting and breakthrough bleeding in weeks 3-4 of your cycle.
G. You Are in Perimenopause
During perimenopause (the ~ 10 years before menopause), you ovarian function starts to decline. The eggs are generally not as good of quality anymore, though some are better than others. Estrogen is being made well some months, and not so well other months. So some months you’ll have a more normal cycle, and other months you can flow quite early, late or heavily.
To some extent this is ‘normal’, as the body is aging and getting ready to leave its reproductive phase. (It’s sad; I know.) But there are ways to ease the transition too.
H. You Have Fibroids or Endometriosis
Fibroids are masses that form in or on your uterus. Estrogen dominance is generally to blame for how these grow in the first place. Then to make matters worse, they respond to the cyclic hormonal changes of your menstrual cycle, and grow and shed like your uterine lining.
This can cause very heavy bleeding and can lead to anemia.
Some women can have a separate condition called endometriosis. Uterine tissue migrates outside the uterus, for example, around the abdomen. When a woman menstruates, endometrial tissue - wherever it is in the body - bleeds.
I. You Have Recently Given Birth or Had a Miscarriage
Birth
After I gave birth to my son, I was shocked by how much bleeding I had for so long. Though everyone generously gave me blankets and baby toys, no one warned me about this!
According to the folks at What To Expect, “the heaviest of the bleeding will last for about three to ten days after labor and delivery and then it should taper off to lighter spotting after pregnancy. You'll see the difference in the color as this starts to happen, from red to pink, then brown, and finally to a yellowish white. Lochia (mix of blood, mucous, tissue) should stop flowing around four to six weeks after delivery.”
I definitely remember bleeding for a least a month. If you continue the bleed heavily after 10 days (like changing a pad every hour), contact your doctor. Even if you had a C-Section, you will still be expelling blood and loch after birth.
Miscarriage
I have never had a miscarriage, but I’ve heard some horror stories from my clients.
If you are less than eight weeks pregnant when the miscarriage occurs, the expelled tissue will look no different from heavy menstrual bleeding. The further along you are in pregnancy, the heavier the bleeding and more severe the cramps.
According to Maricopa OBGYN page,
“During the miscarriage, you may bleed heavily, soaking a pad every 10 minutes. The cramping can be quite uncomfortable.
Although cramping, bleeding and occasional clotting is normal after both a miscarriage and a D&C, you should not be soaking more than 2 pads an hour nor experience worsening, exquisite pain after the uterus has been emptied. These are important symptoms to report to you doctor.
During your recovery, you will continue to bleed, on and off, for up to 3 weeks. Some minor cramping will continue in the next few days also. If bleeding increases or stays bright red, or if you have foul-smelling discharge or a fever or persistent cramping, contact your health care provider.”
J. Uterine and Cervical Cancer
It is possible that heavy bleeding could arise from uterine or cervical cancer. These conditions could involve heavy flow or spotting at random times, or after sex. The odds are that your heavy flow or spotting is due to an item in above list.
Cervical cancer usually will not process to heavy bleeding unless the disease is quite progressed. The best prevention is to practice safe safe and to get a pap smear every 5 years or as directed by your physician. Cervical cancer often develops from certain strains of the Human Papillomavirus (HPV).
Uterine cancer is more comely diagnosed in women over 50 years old, although there are other risk factors such as obesity and a history of irregular cycles. Every year, about 52,000 U.S. women are diagnosed with uterine cancer, according to the National Cancer Institute.
K. Hemophilia
It is possible that you will have heavy bleeding due to a blood clotting disorder. If you are missing clotting factors VIII or IX, you will also experience easy bruising or nose bleeds, and can have very heavy bleeding after childbirth. You will probably have menstrual pain as well. This condition is rare, 1 in 5,000 - 10,000 for type A and 1 in 50,000 - 100,000 in type B, but if you suspect this, especially if there is heavy bleeding in your family, ask your doctor.
3. What Can You Do About Heavy Bleeding?
As I shared above, the most common reason for heavy bleeding is estrogen dominance, so let’s start there for solutions:
A. Avoid Xenoestrogens
Xenoestrogens are synthetic chemicals that look and act like estrogen in your body. When these are present, it’s easy to get into estrogen dominance and heavy periods. The top tips are:
Eat organic
Use all natural cleaning and beauty products
Avoid using plastics for cooking and food storage.
B. Watch your Weight
Estrogens are also made in your fat tissue through a process called aromatization. If you are trying to eat right and exercise but can’t lose weight, avoid xeno-estrogens, check your thyroid, make sure you get a good night’s sleep.
C. Check Your Thyroid
I love Izabella Wentz’s ‘safety theory’ that theorizes that when your body is under stress (emotional, chemical, or pathogenic), it dials down thyroid production as a way to get you to safely hibernate. It’s fascinating. Read about it here.
If you do get your thyroid checked, be sure to do it up right, getting a full thyroid panel and having it interpreted by a functional medicine type practitioner. Jen Wittman of Thyroid Loving Care has some great info on that here.
D. Try Herbs and Supplements
I am not a fan of using supplements unless you have a solid base of good habits, and have checked for other underlying causes. But I will mention a few nice supplements here, and you can check with you doctor if it’s safe for you to use them.
1. Vitex - This herb, that is also called chaste tree berry, seems to benefit communication between your ovaries and your brain, and it’s especially good at increasing progesterone. It may not be as useful for women in their late 40s, and it may not be a fit for everyone, but it has many success stories. It can be taken daily throughout your cycle. Use for 6 months, unless you have an adverse reaction.
2. Di-Indoly Methane (DIM)- DIM is a star at clearing excess estrogen. It’s often used for PCOS (polycystic ovarian syndrome) but it can be useful in most any case of estrogen dominance. For more information, see this blog at NaturoDoc. According to Dr. Holly Lucille, ND, RN, DIM shifts estrogen metabolism to the healthy 2-hydroxy pathway (makes for nice skin) in place of the troublesome 16-hydroxy pathway (makes for heavy periods and cancers).
3. Calcium-D-Glucarate (CDG)-This is one I’ve just learned about recently. CDG also does a great job at clearing spent estrogen from the body. Here’s some cool information on how it works from Dave Asprey at bulletproof.com:
“One of the ways the body gets rid of toxins is through a process called conjugation. During conjugation, toxins are packaged into water soluble compounds called glucuronides. Glucuronides are meant to pass from the liver, to the bile, then to the gut where they are excreted. However, high levels of an enzyme called beta-glucuronide can inhibit this process. This enzyme separates toxins from their conjugate bond and allows them to be reabsorbed. This allows toxins to keep circulating in the body where they make you fat, tired, and weak.
Calcium-d-glucarate prevents beta-glucuronide from disturbing this process. It keeps the toxins bound inside a glucuronide which is then removed from the body. Toxins are most damaging in their free form, which is why you want them to be bound (conjugated) and released from the body. Calcium-d-glucarate inhibits beta-glucuronidase which allows toxins to be removed.”
E. Heal Your Gut
You might be surprised to hear that your digestive tract has anything to do with heavy periods! But it’s so. Your gut is the place where food is broken down into the nutrients you need to make hormones. It’s also the place where used hormones are broken down and expelled. So it needs to be a healthy environment, free of inflammation, full of good bacteria, and moving daily.
This is a big topic to cover, but here are two top tips:
Chew your food and eat a relaxed fashion. Gulping down food while scanning your smartphone does not lead to proper digestion.
Eat a variety of fibers daily/ weekly. Fibers from berries, nuts, seeds and vegetables will fuel the friendly bacteria in your gut. And don’t get stuck eating the same 4-5 things; mix it up for greater bacteria diversity.
F. Try Chinese Medicine
Chinese medicine can be a relaxing way to balance your hormones. Herbal formulas like Bu Zhong Yi Qi Tang, and treatments like moxibustion on your spleen 1 point can stop a heavy flow. Look for a practitioner who specializes in women’s health in your area. If you’re in Portland, Oregon, come check us out at Blue Sky Wellness Studio.
G. Zen Out
A major hormone disruptor is stress. It blocks hormone receptors, raises blood sugar and blocks production of reproductive hormones. The reproductive hormone that goes down first is usually progesterone, and you’ve learned you need that to balance out the estrogen.
My best advice here is to focus on having fun. If you stay connected with friends, go to a delicious meal with your sweetie, or take a work break to visit the sauna (I did this today), it’s hard to stay obsessed with your problems. Problems will always be there, so seize the moment and enjoy life!
H. Seed Cycling
Seed cycling means taking certain nuts and seeds in the first 2 weeks or your cycle, and another type in the second two weeks. The alternating phases support first your estrogen production and then your progesterone production, plus the fiber helps clear spent hormones. I already wrote a whole blog on this topic, which you can access here.
Wow, thanks for sticking with me and reading this very long article on heavy periods! I hope it helps you. If you’d like more in-depth support, we offer private health coaching here.
Bridgit Danner, LAc, FDNP
Founder of Women’s Wellness Collaborative